Information, resources and tools to help you manage your gout symptoms and improve function.
Gout is the most common form of inflammatory arthritis, affecting as many as 1 million Canadians.
Gout can happen when there is too much uric acid in the bloodstream. Uric acid is produced by the breakdown of purines, which are found in the foods we eat.
 Kidneys help to filter out uric acid, which our bodies get rid of through urine. When the kidneys are not able to filter or process uric acid levels at the same rate they are being created, this can cause high uric acid levels to remain in the bloodstream.
Kidneys help to filter out uric acid, which our bodies get rid of through urine. When the kidneys are not able to filter or process uric acid levels at the same rate they are being created, this can cause high uric acid levels to remain in the bloodstream.
Genetics play an important role for those at risk of having gout. Some bodies will breakdown purines into uric acid and be able to excrete excess uric acid more easily than others. Even if two people have the exact same diet and eating habits, one person could have higher levels of uric acid in their bloodstream, and be at an increased risk of developing gout.
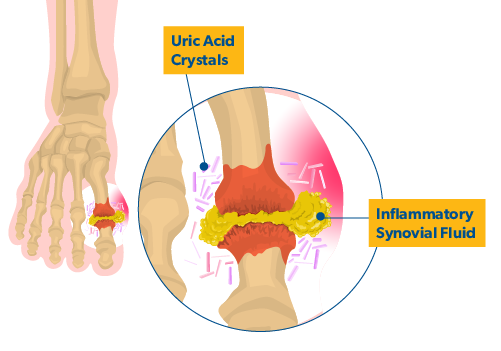
After months to years of sustained high level of uric acid in the bloodstream (usually above 400 µmol/l) the uric acid can leave the bloodstream and form uric acid crystals in joints and soft tissues.
Uric acid crystals in soft tissues are usually found under the skin and form hard bumps with a white chalk-like colour. When they are present, these crystal deposits, called tophi [toe-fi] can usually be seen around the ears and around extensor tendons, which are found in hands and feet. Uric acid crystals in joints can be responsible for gout attacks.
Click on the cards below to learn about gout and how to manage it to live well.

Online Learning Guides
Learning modules to help you cope and thrive when living with gout.
View More Guides

Arthritis Talks Webinars
Arthritis Talks webinars on the latest guidance direct from arthritis experts to help you get more out of life with gout.
Understanding Gout
In this Arthritis Talks webinar rheumatologist and gout expert, Dr. Jean-Philip Deslauriers, delves into everything you need to know...
In this Arthritis Talks webinar rheumatologist and gout expert, Dr. Jean-Philip Deslauriers, delves into everything you need to know about gout.
Gout Self Defence: Preventing Painful Attacks
Dr. Alexa Smith discusses gout at a public forum in Saint John presented by The Arthritis Society on November 18th, 2015. Sponsored...
Dr. Alexa Smith discusses gout at a public forum in Saint John presented by The Arthritis Society on November 18th, 2015. Sponsored by Takeda Canada, Inc.
Eat Smart for Arthritis
We know eating well can make a big difference when you live with arthritis. But figuring out what works best for you may feel...
We know eating well can make a big difference when you live with arthritis. But figuring out what works best for you may feel overwhelming. In this webinar registered dietician Lalitha Taylor examines the role of food in managing arthritis symptoms and answers your questions about arthritis and nutrition.
View More Webinars
View All Arthritis Types (A - Z)