Information, resources and tools to help you manage your osteoarthritis symptoms and improve function.
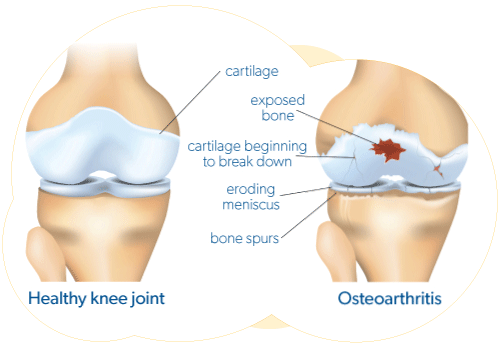 Osteoarthritis (OA) is the most common type of arthritis. It affects more Canadians than all other forms of arthritis combined. Osteoarthritis is a progressive disease of the whole joint that leads to the breakdown of joint cartilage and the underlying bone. (Cartilage is the tough elastic material that covers and protects the ends of bones).
Osteoarthritis (OA) is the most common type of arthritis. It affects more Canadians than all other forms of arthritis combined. Osteoarthritis is a progressive disease of the whole joint that leads to the breakdown of joint cartilage and the underlying bone. (Cartilage is the tough elastic material that covers and protects the ends of bones).
Joints require the body to regularly repair and replenish damaged tissues. Damage to joint tissues can occur through the normal function of a joint. When the body is not able to keep up with the repair process, or if there is too much tissue that requires repair to take place, osteoarthritis may begin to develop. For most people, this damage can occur when otherwise healthy joints are exposed to heavy workloads over a long period of time. However, for some people whose joints are formed differently or who have experienced a previous joint injury, even regular workloads can accelerate joint damage. Being overweight or obese is also a risk factor for developing osteoarthritis since additional body weight can cause significant stress on weight-bearing joints.
There is currently no cure for osteoarthritis, however, there are ways to manage the symptoms and how you function in daily life. This can include a combination of self-management strategies, medications, treatment by healthcare professionals specializing in orthopedic care and, for severe osteoarthritis, possibly joint replacement surgery.
Treatment
While the underlying process of osteoarthritis (OA) cannot be reversed, the symptoms can often be relieved or significantly improved with self-management strategies (e.g., therapeutic exercise, physical activity, weight management) and medications. Surgery is reserved for severe symptoms that fail to improve with these strategies. The two main goals of osteoarthritis treatment are to control your pain and improve your ability to function.
Therapies
The following healthcare professionals have advanced training from a university and are registered to practice by their provincial/territorial association:
Physiotherapy
 A physiotherapist (PT) can develop an individualized program designed to help you increase your strength, flexibility, range of motion, and general mobility and exercise tolerance through a wide variety of therapeutic treatments and strategies. These include exercise plans, physical interventions, and relaxation, in addition to advising you on other techniques for reducing pain and increasing your overall quality of life. PTs can recommend foot orthotics, knee braces and hand splints.
A physiotherapist (PT) can develop an individualized program designed to help you increase your strength, flexibility, range of motion, and general mobility and exercise tolerance through a wide variety of therapeutic treatments and strategies. These include exercise plans, physical interventions, and relaxation, in addition to advising you on other techniques for reducing pain and increasing your overall quality of life. PTs can recommend foot orthotics, knee braces and hand splints.
Occupational therapy
An occupational therapist (OT) can look at what you do in a day and develop a program to help lessen your symptoms and improve your function. An OT can do a home or workplace assessment to identify ways to protect your joints and can recommend tools and aids to help you conserve energy and improve your independence. Examples include use of a cane and raised seats to decrease stress on your hip and knee joints; use of wide gripped tools and utensils to decrease stress on your hand joints; or the use of shoehorns or buttonhooks to help with dressing. OTs can also recommend foot orthotics, knee braces and hand splints.
Other therapies often used to help manage osteoarthritis symptoms include:
- Acupuncture is a traditional Chinese therapy that is said to help restore the body’s energy flow (Qi) by inserting thin needles into areas of the body that follow energy lines, known as meridians. Acupuncture is sometimes used to alleviate pain and treat various physical and mental health conditions. Acupuncture has been shown to yield anti-inflammatory effects and regulation of immune system function. However, there is limited research evidence regarding its impact on arthritis symptoms. Because of its low risk of harm, acupuncture combined with standard arthritis medication strategies may be beneficial in reducing pain and improving quality of life.
- Massage of muscles and other soft tissues by a registered massage therapist, may help provide short-term relief of stiffness and pain. Other potential benefits include a reduction in stress and anxiety as well as improved mobility and overall function of the joints. However, there currently isn’t enough research evidence to suggest massage should be recommended for everyone managing osteoarthritis symptoms. Always consult your family doctor or rheumatologist to see if massage therapy is safe and appropriate for your form of arthritis.
Drug-Free Pain Management Tool: Learn about drug-free alternatives to arthritis pain management.
Inform your healthcare provider of any complementary and alternative therapies you are taking, receiving or would like to try. Your health-care provider can offer valuable advice about these treatments, especially how they may affect other medications and treatments.
Complementary Therapies Guide for Arthritis: Learn more about how to choose complementary therapies.
“Your care plan should involve education about osteoarthritis, lifestyle changes such as increasing physical activity, eating healthier, weight-loss, and doing therapeutic exercises.” – Physiotherapist
Osteoarthritis medications
Medications for osteoarthritis focus on helping to manage pain and improve joint function. For mild symptoms that come and go, you may benefit from using medication as needed. For stronger symptoms, you may require regular use of medication. The best treatment is what works for you – so speak with your doctor and/or pharmacist about what kind of medications are most appropriate for you.
Medications that may help relieve pain from osteoarthritis come in topical forms (e.g., creams or rubs), pill forms, oils, and injections. Common medications used in osteoarthritis are described below:
- Topical treatments

- Topical treatments include non-steroidal anti-inflammatory drug (NSAID) creams and capsaicin cream.
- Corticosteroid injections
- These injections may relieve symptoms for several weeks to months. Most people tolerate them with few side effects.
- Acetaminophen
- Acetaminophen has fewer side effects than other pain medications. It is important to stick to the recommended dose, as a higher dose may cause liver damage.
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- If other treatments do not relieve your arthritis pain, you are advised to speak with your pharmacist or doctor about the safety of NSAIDs for you. NSAIDs may reduce pain and inflammation in osteoarthritis. There are a variety of over-the-counter NSAIDs which include ibuprofen and naproxen sodium. Stronger NSAIDs are available by prescription. If, after checking with your doctor, you are safe to use an NSAID medication, it may work better for your arthritis pain if you take it in combination with acetaminophen.
- Duloxetine
- This medication has been used to treat a number of chronic pain conditions including osteoarthritis, nerve disorders and fibromyalgia. Duloxetine may be recommended if you do not respond to or cannot tolerate acetaminophen or NSAIDs. It may have added benefit if you are also experiencing depression.
- Other injections
- Viscosupplementation (hyaluronic acid) injections are not routinely recommended for treatment of osteoarthritis due to limited benefits, risk of side effects and high costs of the various agents available. There is limited evidence to support platelet-rich-plasma injections for knee osteoarthritis. Given the cost of these injections and limited evidence, corticosteroid injections are often the first choice.
- Medical cannabis
- Increasingly, many people with arthritis are exploring medical cannabis as a treatment option for their arthritis. While cannabis can’t cure arthritis or slow disease progression, some people report that it helps to alleviate their symptoms of pain, inflammation and anxiety. There is currently limited evidence available on the efficacy of medical cannabis use for arthritis symptoms, though further research is underway. Visit our Medical Cannabis page to learn more.Medical cannabis may not be covered by all drug plans. It is important to check with your insurer about coverage and annual limits. Medical cannabis can be claimed as a medical expense on taxes if obtained with a medical authorization document.
- Opioids
- Opioids are not considered an appropriate first-line treatment option for osteoarthritis, and their potential harms have been shown to outweigh any benefits in treating pain from osteoarthritis. Opioid use can also lead to a pain over-sensitization, where regular use can cause your body to become more sensitive to pain and less responsive to opioid medications. Opioid use can also increase the risk of developing a physical dependency on the medication, which can cause other health concerns and make it difficult to stop taking this type of medication. Long-term pain relief for osteoarthritis is best achieved through a combination of therapeutic exercise and drug-free pain management, and if needed, other forms of medication discussed with your doctor.
Surgery for osteoarthritis
 When osteoarthritis becomes severe and other therapies are not working, surgery may be considered. The most common surgical procedures for osteoarthritis include hip and knee replacements, but other joints may be partially or fully replaced surgically as well.
When osteoarthritis becomes severe and other therapies are not working, surgery may be considered. The most common surgical procedures for osteoarthritis include hip and knee replacements, but other joints may be partially or fully replaced surgically as well.
Joint replacement surgery can be performed at any age, but is usually reserved for patients with advanced arthritis. The decision to undergo surgery depends on the amount of pain and disability your arthritis is causing, as well as the risks and benefits of surgery. Surgery may not be helpful for patients who only have mild arthritis, even if they have significant pain. This should be discussed further with your doctor.
Self-Management
The first line of treatment for osteoarthritis involves a number of steps you can take on your own under the guidance and supervision of a heal
thcare professional. These include patient education, developing a self-management plan, therapeutic exercise, physical activity and weight management, if appropriate (HQO, Quality Standard: Osteoarthritis, 2018, OARSI Guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis, 2019).
An important first step is to become informed about osteoarthritis and what you can do to manage symptoms on your own. This is referred to as self-management. You can learn ways to cope with arthritis symptoms and make lifestyle changes that may reduce pain and improve joint function and your mood.
Lifestyle changes such as increasing physical activity and exercise and reducing excess body weight can have the greatest effect on osteoarthritis. Developing relaxation and coping skills can help you maintain balance in your life, giving you a greater feeling of control over your arthritis and a more positive outlook.
Physical activity
 A common misconception is that a painful joint requires rest. However, not enough movement can cause muscle weakness, worsening joint pain and stiffness. Light or moderate physical activity protects joints by strengthening the muscles around them, increasing blood flow to the joint and helping promote normal joint regeneration. Physical activity can also improve your mood and lessen pain.
A common misconception is that a painful joint requires rest. However, not enough movement can cause muscle weakness, worsening joint pain and stiffness. Light or moderate physical activity protects joints by strengthening the muscles around them, increasing blood flow to the joint and helping promote normal joint regeneration. Physical activity can also improve your mood and lessen pain.
Physical activity is any movement that increases your heart rate through activation of your muscles, while exercise is considered a structured, planned, repetitive and purposeful activity with the goal of improving or maintaining a component of physical fitness. The Canadian Physical Activity Guidelines are an evidence-based set of general recommendations detailing appropriate levels of activity for people of different ages. Using these guidelines to increase your physical activity, even in small increments, may help relieve arthritis symptoms and improve your daily functioning.
Physical activity strengthens the muscles and connective tissues around your joints, helping support joints that have been damaged by arthritis. Physical activity includes all those activities that you do as a part of everyday life – such as vacuuming the house, walking to work, and even gardening. These kinds of activities can be very beneficial for your joints, and can help you maintain and improve your mobility.
Canadian 24-hour Movement Guidelines
The Canadian 24-hour Movement Guidelines are an evidence based set of general recommendations detailing appropriate levels of activity for people of different ages.
Exercise
 Exercise is physical activity that involves heavier, repetitive actions, and is designed to improve or maintain physical fitness. Activities like lifting weights, walking on a treadmill, or taking a yoga class are different forms of planned motion that specifically work to improve strength, endurance or flexibility.
Exercise is physical activity that involves heavier, repetitive actions, and is designed to improve or maintain physical fitness. Activities like lifting weights, walking on a treadmill, or taking a yoga class are different forms of planned motion that specifically work to improve strength, endurance or flexibility.
Participating in a properly designed exercise program is a great way to help alleviate the discomfort caused by arthritis. Therapeutic exercise can reduce pain and fatigue, improve mobility and overall fitness. It can also help improve mood and state of mind by allowing you to actively participate in your own treatment.
Exercises targeted for your joints may have added benefit. A qualified professional, such as a physiotherapist, can work with you to develop a progressive exercise program that is customized for you. GLA:D Canada’s evidence-based education and exercise programs also offer exercise plans designed for hip and knee osteoarthritis.
There is conflicting evidence about the possibility of harm from high-impact exercise, such as running, soccer or tennis, so you will need to determine what activities your body can tolerate and consult with your doctor. You may have to modify or swap out an activity if it worsens your joint symptoms, though there are also many ways to participate in adaptive sports that might be an option for you.
It is recommended to rest your joint when you experience a flare of joint pain and/or your joint is swollen and hot. However, it is still important to keep doing range of motion exercises during these times.
What types of exercise are recommended for osteoarthritis?
- Therapeutic exercise
- Often developed with the help of a healthcare professional, this type of exercise is a set of planned motions designed to help you improve strength, flexibility, fitness and balance. It is goal oriented, structured physical activity that includes awareness of posture and alignment. Therapeutic exercise outcomes include developing ‘muscle memory’ by training your joints and muscles to move in healthy patterns, strengthening your muscles, as well as improving balance and agility.
- Range of motion exercise
- These are also called stretching or flexibility exercises. Exercises that keep your joints moving can reduce pain and stiffness. To achieve the most benefit, these exercises should be done daily.
- Strengthening exercise
- Exercises that maintain or increase muscle tone and protect your joints. These resistance-based exercises include weight-training movements done with a set of free weights, your own body weight, resistance bands or weight machines. For example, thigh (quadriceps and hamstring muscles) strengthening is recommended for people with knee osteoarthritis. The frequency of strengthening exercises should be discussed with your doctor or physiotherapist.
- Endurance exercise
- Exercises that strengthen your heart, give you energy, control your weight and help improve your overall health. Examples include walking, swimming and cycling. Activities like Tai Chi and Yoga that combine muscle strengthening, flexibility, and balance exercises can be beneficial in the management of osteoarthritis. These exercises can also be meditative, promoting relaxation and increasing your capacity to cope.
Tai Chi & Yoga
Activities like Tai Chi and Yoga that combine muscle strengthening, flexibility, and balance exercises can be beneficial in the management of osteoarthritis. These exercises can also be meditative, promoting relaxation and increasing your capacity to cope.
- Tai Chi: This ancient Chinese martial art is a combination of movements performed in a slow, focused manner. Though it has many variations and styles, Tai Chi is a low-impact exercise and is reminiscent of both yoga and meditation. Tai Chi could improve pain and physical function in some people as well as alleviate depression and contribute to improved quality of life.
- Yoga: Numerous studies have shown the benefits of yoga for stress and anxiety. The practice of controlled breathing, simple meditation and stretching can improve a person’s state of mind and help them better manage pain. Regular yoga under the guidance of a certified instructor can also increase general health and energy levels. (NOTE: In some cases, people living with arthritis should avoid strenuous yoga routines, such as Bikram and power yoga.) Our 20-Minute Warm-Up for the Joints video is a great place to start.
Many low-impact exercise options can benefit people living with arthritis. For example, water therapy and swimming can help with pain and mobility. The resistance of the water can help strengthen your muscles while the buoyancy helps take some of the weight off painful joints. Consult your health-care provider to determine which exercises are right for you and your particular condition.
How much exercise is recommended for people with osteoarthritis?
Any increase in your physical activity or exercise may help if you are not currently active. However, the frequency, intensity, type and duration of activity will vary from person to person. A gradual increase in exercise is recommended, with an eventual target for adults of 150 minutes of moderate-to-vigorous exercise per week, in sessions of 10 minutes or more (if tolerated). If you are not currently active, start with light activities, such as walking, and attempt to increase your speed and/or distance over time.
Symptoms and Diagnosis
What are early signs and symptoms of osteoarthritis?
Osteoarthritis (OA) usually progresses slowly over a period of months or years. Early on, osteoarthritis symptoms tend to come and go. Over time, as damage accumulates, symptoms can become more constant, occurring at rest and disturbing sleep. The good news is that symptoms can improve with treatment, even if the disease process itself is unchanged. Symptoms may be experienced in the joint or outside of the joint as well.
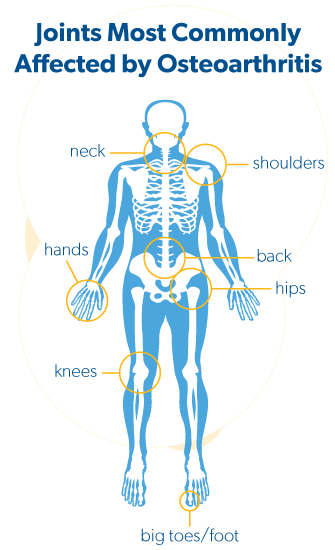
Osteoarthritis can affect any joint, but most commonly affects the knees, hips, big toes, hands and spine. Many people are affected by osteoarthritis in more than one joint. Osteoarthritis affects everyone differently, however common symptoms include joint pain, aching, morning stiffness lasting less than 30 minutes, reduced range of movement in the affected joint(s) and possibly swelling. The symptoms may come and go, but the intensity of pain can increase over time since osteoarthritis progresses over time.
Use the Arthritis Symptom Checker to find out if it could be arthritis. It’s better to know.
Common osteoarthritis joint symptoms include:
- Joint pain
- Your joint may hurt during heavy use, and improve with rest. As the disease progresses, the pain may be triggered by increasingly ordinary activities and may become unpredictable, occurring at rest and during sleep. The pain you feel may not necessarily match the degree of arthritis seen on an x-ray. Pain is a complicated process affected by what is happening inside your joint as well as factors outside of your joint, such as surrounding muscle strength, genetics, physical activity, sleep and mood.

- Your joint may hurt during heavy use, and improve with rest. As the disease progresses, the pain may be triggered by increasingly ordinary activities and may become unpredictable, occurring at rest and during sleep. The pain you feel may not necessarily match the degree of arthritis seen on an x-ray. Pain is a complicated process affected by what is happening inside your joint as well as factors outside of your joint, such as surrounding muscle strength, genetics, physical activity, sleep and mood.
- Joint stiffness
- Your joint may be stiff after not moving it for a while, such as when you wake in the morning or sit for a long time. This stiffness usually lasts 30 minutes or less. If you find it lasting significantly longer, check with your doctor.
- Joint swelling
- You may notice an increase in the size of affected joints. This can be from an increase in fluid in the joint (inflammation), or from a bony outgrowth (often found in affected finger joints and big toes).
- Joint crepitus
- A noticeable grinding sensation or notice a creaking sound when the joint moves.
- Joint instability
- Joints like the knee or hip may feel like they are giving way or buckling.
- Joint dysfunction
- The joint does not function as well as it should. This can be due to pain or reduced movement of the affected joints:
- Hands – You may have difficulty with fine motor activities, such as doing up buttons, writing with a pen, or gripping door handles.
- Hips – You may have difficulty with daily activities like walking, getting in or out of a car, or putting on your shoes.
- Knees – You may have difficulty with activities like walking, getting up from a chair, squatting, kneeling or climbing stairs.
- Shoulder – You may have difficulty putting on a shirt or jacket, sleeping on your side, or holding items that require sustained shoulder movement such as using a hair dryer or a steering wheel while driving.
- Neck – You may experience difficulty with using a laptop or computer monitor for extended periods of time, quick jarring movements, finding a comfortable position to sleep in, or positions that cause you to tilt your head forward, such as when using a smart phone.
- Back – You may experience stiffness or pain when going about daily tasks, especially when standing, sitting or walking for long periods of time, bending forward to pick up items or put on shoes, or performing activities like vacuuming, raking leaves or shovelling snow.
- Foot and ankle – You may have difficulty walking or feeling unsteady on your feet, especially when on uneven ground or on stairs. Daily activities such as grocery shopping, running errands, standing for meal prep, or performing housekeeping may be challenging due to standing or walking for extended periods of time.
- The joint does not function as well as it should. This can be due to pain or reduced movement of the affected joints:
Osteoarthritis symptoms outside the joint may include:
 Sleep disruption
Sleep disruption
Osteoarthritis symptoms may wake you up in the night, which in turn can make your symptoms feel worse, and reduce your ability to cope.
Altered mood
Osteoarthritis symptoms can impact your mood, sometimes causing you to feel irritable, or have less patience than usual. Mental health concerns, including depression and anxiety are also more common in people living with chronic pain, and can in turn worsen pain and negatively impact your overall health.
Fatigue
It is common for people with severe pain from osteoarthritis to experience high levels of extreme tiredness, or exhaustion.
Quality of life
Osteoarthritis symptoms can make it harder for you to keep up with the activities and relationships that make your life enjoyable, affecting your overall quality of life and your ability to do things you want to do.
Pain sensitization
Some people with osteoarthritis may experience more intense pain symptoms due to a process called pain sensitization, which happens when the central nervous system processes pain in an atypical way. It may feel like the ‘volume knob’ on your pain system has been left turned up like a radio stuck on ’loud.’ As a result, you may feel exaggerated pain in response to a painful trigger, pain in response to a non-painful trigger such as light touch, or ongoing pain in the absence of any trigger.
Your feelings of pain may extend beyond the boundaries of the joint and become widespread. For those affected by osteoarthritis of the spine, for example, you may also experience nerve symptoms such as tingling and shock-like sensations. See your doctor to check if these symptoms are from your arthritis, or from another cause.
It’s really important to understand that it is possible to ‘turn the volume down’ using pain management techniques and activities such as regular exercise, optimizing sleep, and practicing stress-reduction and mindfulness. It can often take time to notice changes in pain when starting new management techniques. Medications that target the central nervous system may also be beneficial. Your healthcare provider can help to guide you in this process.
How is osteoarthritis diagnosed?
 There is no single test for osteoarthritis. A diagnosis can be made based on your symptoms and a physical examination of your affected joint(s).
There is no single test for osteoarthritis. A diagnosis can be made based on your symptoms and a physical examination of your affected joint(s).
For people over the age of 40 who have symptoms typical of osteoarthritis, a diagnosis can be made based on a clinical assessment. X-ray or MRI is not typically part of the diagnostic process, unless it is being used to rule out a potential injury.
However, an x-ray or MRI may be ordered if you have not been responding to your treatment or management plan, or if you and your doctor are planning a surgery where imaging would be helpful. If an x-ray or MRI is ordered, it is important to know that symptoms of osteoarthritis do not always match what is found on imaging. For example, in the early stages of osteoarthritis, an x-ray or MRI may not reflect the symptoms you are experiencing, and later in the disease process, the damage shown on imaging may appear more severe than the pain or other symptoms you feel.
What are the risk factors for osteoarthritis?
Risk factors that may increase your chances of developing osteoarthritis include the following:
 Age: The risk of osteoarthritis increases with age. However, it is not an inevitable part of aging. Many people age without having osteoarthritis symptoms.
Age: The risk of osteoarthritis increases with age. However, it is not an inevitable part of aging. Many people age without having osteoarthritis symptoms.- Sex: Females are more likely to develop osteoarthritis than males. Note: Information is based on self-reported sex identification.
- Family history: Genetics can contribute to the development of osteoarthritis, but just because your family member has osteoarthritis does not mean you will get it.
- Excess body weight: Carrying extra body weight increases your chance of getting osteoarthritis in several ways. Excess weight puts more stress on weight-bearing joints such as your feet, knees, hips and spine, and increases your risk of injury as well as the rate of joint degeneration. In addition, fat tissue can release substances in your body that can increase joint inflammation.
- Joint injury: Osteoarthritis can occur in joints that have been affected by a previous injury, which could have occurred through sport or an accident.
- Occupations: People who repeatedly experience stress on a particular joint or who perform heavy physical labour may also be at greater risk of developing osteoarthritis. Examples include dancers, heavy machinery operators and construction workers.
- Joint misalignment / deformity: Some people who are born with or develop malformed joints are at greater risk of osteoarthritis.
- Muscle weakness: Weakness of supporting structures around the joint such as muscles and ligaments can increase the risk of osteoarthritis.
- Sedentary lifestyle: A lifestyle that involves very little to no physical activity can increase your risk of osteoarthritis.
 What is the osteoarthritis patient journey?
What is the osteoarthritis patient journey?
A patient journey is the sequence of events that a person with osteoarthritis experiences, from the first signs of symptoms to diagnosis and later to treatment and management. Not all steps will be the same for everyone, but it can give you an idea of what you may expect and how to effectively manage your osteoarthritis.
How common is osteoarthritis?
Osteoarthritis is the most common form of arthritis, affecting more than four million Canadians (one in seven).
These numbers are expected to increase as the population ages and grows. Osteoarthritis is more common in females than in males, and becomes more common as age increases.
Among people with osteoarthritis who experience joint pain, the most commonly reported painful joint site is the knee, followed by the hand, back, hip, and shoulder. It is common for osteoarthritis to affect multiple joints. As many as four in five Canadians with osteoarthritis report having pain in two or more joint sites, and more than 40 per cent report having pain in four or more joint sites.
Activities
Low Load Activities for Osteoarthritis
Optimal Set-Up and Modifications
If your hip and/or knee pain is much worse on stairs or with longer walks, consider starting with activities that put less weight load on your joints, such as: cycling, walking with walking poles, Tai Chi, yoga, Pilates, and water-based activities like aqua fit, swimming, or pool walking.
Cycling
Cycling is frequently recommended because there is much less load through your hip, knee & ankle joints as your weight is supported on a seat, allowing you to do more with less discomfort. Cycling provides a low-impact, high-intensity heart/lung workout, builds leg muscle strength and endurance that are often weakened by arthritis, and helps maintain hip and knee movement.
If you prefer to use a stationary bike there are 2 types to choose from: upright and recumbent. Choose the one you find more comfortable, both will provide you with health benefits.

Setting up the bike (indoor or outdoor) in the right position will make you more comfortable, limit your chance of injury, and allow you to get the most from your workout.
- Seat position – your knee should be slightly bent and in a relaxed position, when the pedal is furthest away from you no matter what type of bike you are on. If your knee is bent too much, you may experience more discomfort in your lower back, hips & knees. On the other hand, you don’t want to be reaching for the pedals.
- Handlebar height (on an upright bike) – with your hands on the handlebars, your elbows should be slightly bent so your neck, shoulders, arms, and hands are relaxed.
- Pedal straps hold your feet in place on the pedals, allowing you to push down and pull up in a circular motion. This gives you a better workout (by using more muscle groups) and places less load on the knees. Straps should be snug; if your feet feel numb, they are too tight.
Walking with Walking Poles
The use of walking poles has become quite popular as they can help with balance, reduce limping, offload the lower extremity joints and engage more muscles of the arms & legs to provide a greater cardio workout. A number of community groups offer free trial sessions that show you how to set up and use the poles properly and go for a walk. To find a group near you, look up Nordic walking or pole walking.

To measure the height of the pole, have your walking shoes on and bend your elbow to a 90-degree angle. With the pole straight up from the ground, the handle should be at the height of your hand. There are many types of poles available, with or without hand straps. You may want to try different types to see what you prefer. If you are walking on hard surfaces, make sure your poles have rubber tips to absorb shock. Use the poles in the same way that you walk, by moving one arm forward with the opposite leg.
Tai Chi, Yoga and Pilates
Tai Chi, yoga and Pilates are often referred to as mind-body activities. They focus on body position and alignment to produce precise and optimal movement patterns also known as neuromuscular training. Optimal movement patterns reduce abnormal load on the joint and result in less pain. These practices focus on the alignment of knee tracking over the 2nd toe while bending and straightening in standing position, keeping your knees from collapsing inward. This alignment is also important in everyday activities like rising from a chair, doing stairs, bending down and riding a bike. These practices also work on single leg balance, requiring strength of your core and buttock muscles to keep your pelvis level and balanced, which can be important for walking without a limp.
Getting up and down from the floor may be hard. Using a wall, chair or aerobic step can help you get up. Doing your exercises seated on an aerobic step or stool rather than on the floor may be easier. If kneeling on the floor is uncomfortable, you can either kneel on or over a rolled-up towel or yoga mat positioned under your upper shin.
Water-Based Activities
Water supports a large proportion of our body weight, reducing pressure on the joints and making it much easier to move for people that have trouble with weight bearing activities. The deeper the water, the more offloading occurs. Walking in water can be a good exercise and much easier than on land. Swimming and aquafit can also be fun. Some people with hip and knee arthritis may have trouble with leg movements like the breast stroke or eggbeater, so should try using another movement like the flutter or scissor kick.

Modifying Activities for Osteoarthritis
Activities That May Increase Your Pain & How To Modify Them
Activities |
Examples |
Modifications |
|
High Impact
|
|
|
|
Twisting
|
|
|
|
Forceful end of movement
|
|
|
|
Getting down to floor or up
|
|
|
|
Kneeling*
|
|
|
* Kneeling will not cause knee damage, but it may be uncomfortable if you have knee arthritis. You can either kneel on a firm, soft surface like a rolled-up towel or position a towel beneath your upper shin. For gardening, you may like a garden kneeler seat with side handles that help you get up from ground level.
This resource was made possible through an educational grant from:

Resources for Clinicians
Resources, tools and guides for healthcare professionals to help identify and case ma
nage patients with osteoarthritis.
- Osteoarthritis Tool
(Arthritis Alliance of Canada, Centre for Effective Practice, and College of Family Physicians of Canada)
The Osteoarthritis (OA) Tool has been developed for primary care providers who are managing patients with new or recurrent joint pain consistent with OA in the hip, knee or hand. This tool will help clinicians identify symptoms and provide evidence-based, goal-oriented non-pharmacological and pharmacological management while identifying triggers for investigations or referrals. - Osteoarthritis Quality Standards: Care for Adults with Osteoarthritis of the Knee, Hip or Hand
(Health Quality Ontario)
The quality standard focuses on the assessment, diagnosis, and management of [osteoarthritis] for people across all health care settings and health care professionals. - OARSI Guidelines for the Non-Surgical Management of Knee, Hip and Polyarticular Osteoarthritis
(Osteoarthritis Research Society International)
These guidelines serve to “update and expand upon prior Osteoarthritis Research Society International (OARSI) guidelines by developing patient-focused treatment recommendations for individuals with Knee, Hip, and Polyarticular osteoarthritis (OA) that are derived from expert consensus and based on objective review of high-quality meta-analytic data. - The American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Osteoarthritis of the Hand, Hip and Knee – 2019
(American College of Rheumatology/Arthritis Foundation)
An evidence-based guideline for the comprehensive management of osteoarthritis (OA) - Managing Hip & Knee Osteoarthritis in Canada
(Bone & Joint Canada)
A report on the 2019 national meeting of Bone & Joint Canada on Managing Hip and Knee OA: From Diagnosis to Surgery
Contributors
This osteoarthritis resource was reviewed in February 2021 with expert advice from:
Dr. Sarah E. Ward, MD, FRCSC
Orthopaedic Surgeon, Division of Orthopaedic Surgery
St. Michael’s Hospital
Assistant Professor, Department of Surgery
University of Toronto
Members of the Canadian Arthritis Patient Alliance Steering Committee, including:
- Linda Wilhelm
- Janet Gunderson
- Therese Lane
- Louise Crane
This resource was made possible through unrestricted educational grants from:
 |
 |
 |
 Just as there is no single definition of a healthy body, there is no single definition of a healthy weight – it’s unique for each individual based on body composition, age, sex, lifestyle and other conditions. The best way to determine an appropriate weight for you is to consult with a healthcare professional.
Just as there is no single definition of a healthy body, there is no single definition of a healthy weight – it’s unique for each individual based on body composition, age, sex, lifestyle and other conditions. The best way to determine an appropriate weight for you is to consult with a healthcare professional. Cold
Cold Heat
Heat Developing relaxation and coping skills can help you maintain balance in your life, giving you a greater feeling of control over your arthritis and a more positive outlook. Relaxing the muscles around a sore joint reduces pain. There are many ways to practice relaxation. Try meditation or deep breathing exercises. Listen to music or relaxation tapes. Imagine or visualize a pleasant and restful activity, such as lying on a beach.
Developing relaxation and coping skills can help you maintain balance in your life, giving you a greater feeling of control over your arthritis and a more positive outlook. Relaxing the muscles around a sore joint reduces pain. There are many ways to practice relaxation. Try meditation or deep breathing exercises. Listen to music or relaxation tapes. Imagine or visualize a pleasant and restful activity, such as lying on a beach.